Sperm diagnostics
General information on sperm diagnostics
Even a simple physical examination, consisting of observing the secondary sexual characteristics (e.g. physique, hair growth) and palpation of the testicles can give the examiner initial suspicions about the cause of sterility. However, the most important examination is certainly the sperm examination (seminogram) and, if necessary, the examination of the SFI (sperm fragmentation index).
Seminogram
The examination of semen quality includes the determination of sperm concentration, sperm motility and sperm morphology (% normal sperm shape).
HALO test, SCSA test
Further investigations, in which the presence of molecule breaks in the genetic material in the sperm heads are determined, provide additional information.
Seminogram
The basis for the diagnosis of possible male fertility problems is the seminogram.
Here, various parameters of the ejaculate (seminal fluid) are examined. However, the most important ones are:
- quantity,
- pH value,
- Sperm concentration (in millions of sperm/ml),
- Morphology (percentage of normally formed sperm cells in %)
- Motility (mobility in %).
Standard values according to the specifications of the World Health Organization (WHO criteria):
- Volume 2.0 ml or more
- ph 7.2-8.0
- Sperm concentration >=20 million/ml
- Total sperm count >=40 million per ejaculate
- Motility (movement) >=50 % with forward progression or >=25 % rapid linear motion
- Morphology >=30 % with normal shape
Additionally, assessed are:
- Leukocytes <=1 million/ml
- MAR test < 10 % sperm with adherent particles
- Liquefaction time 30 minutes, max. 1 hour
- Smell chestnut blossom
Further investigations, if necessary:
- Percentage of living sperm 75% or more vital cells that do not absorb dye in the eosin test
Note:
The morphology is often judged by the so-called ” Krueger-strict criteria” or “strict criteria”. According to these criteria, the proportion of malformed sperm can be as high as 85%, and still be considered normal.
The results of seminograms are subject to strong fluctuations , therefore at least 2 (better 3) months should pass between the examinations. The testicles need about this time to form new sperm cells. No less than 3 and no more than 5 days of sexual abstinence should be observed before the examination.
From the differentiated microscopic analysis of sperm quality, it is unfortunately not always possible to obtain an exact evaluation of fertility (fertility prognosis) for men.


SCSA test, HALO test
Although the seminogram is the simplest examination, it only gives partial information.
More and more international studies in the indicate that the proportion of sperm with chromosomal breaks within their genetic material can be of great importance, both for their ability to be fertilized and, for example, for the risk of miscarriage. However, this so-called fragmentation index (FI) cannot be detected by a normal seminogram (microscopic examination of sperm quality).
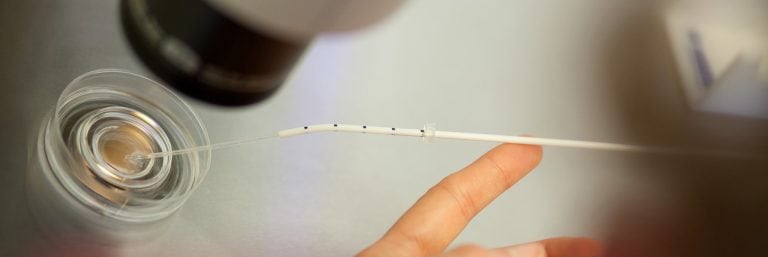
The HALO or SCSA test (sperm chromatin structure assay) offer the possibility to determine the fragmentation index. The additional knowledge of the sperm fragmentation index can be helpful in carrying out a suitable fertility treatment. Thus, a (possibly retrospectively as a less promising) month-long therapy can be avoided. One reason for this is the occurrence of breaks in the genetic material in the sperm, so-called fragmentation.
Up to 25% of men with normal seminogram findings have a high proportion of sperm cells with fragmentation. In these cases, treatments such as transfer of the sperm into the uterine cavity (insemination) or test tube fertilization (IVF/ICSI) may be advisable. Since the breaks in the genetic material cannot be detected by the “normal” seminogram, an additional examination is necessary, the so-called SCSA test or the HALO test. We carry out the HALO test because it is less complicated and cheaper than the SCSA test.
The HALO test offers the possibility to recommend an individualized therapy. This may save time and costs.
The cost of the HALO test amounts to 160.00 Euro. The examination is not yet reimbursed by either statutory or private health insurance companies.
The DNA Fragmentation Index (DFI) provides information on the chances of success of the various treatment methods, whereby only the sperm cells are evaluated in the assessment:
DFI 0 – 15 %:
Pregnancy seems to be possible in a normal way.
DFI 15 -25 %:
Pregnancy is possible by normal means, but the time to conceive may be prolonged. If you have wanted to have children for a longer period of time, you should at least consider insemination therapy (sperm transfer). In the case of additional disorders in the woman and in older women, IVF (in vitro fertilization) is advisable.
DFI > 30 %:
Pregnancy by normal means or insemination seems unlikely. The success rate can be improved by IVF (in vitro fertilization, test tube fertilization).
DFI > 50 %:
Pregnancy with IVF is unlikely, intra-cytoplasmic sperm injection (ICSI) offers better chances.
DFI > 60 %:
Very low success rates; only chance with ICSI or donor sperm.
The recommendations listed here are based on the studies of various research groups in recent years and are only recommendations.